In this newsletter I am continuing the “All Diseases Begin In The Gut” series. This time I am looking at a common gut issue called “leaky gut” or “gut permeability” that in itself triggers a number of health issues including:
- Food intolerances and allergies
- Inflammation, pain and arthritis
- Autoimmune diseases
- Skin issues
- IBS and other gut problems
- Even stress, anxiety and depression states
If you suffer any of these then healing your gut may help you and scientific studies have shown this.
Understanding Leaky Gut or Gut Permeability
The gut is a complex organ responsible for breaking down food in the stomach and absorbing nutrients into the body in the small intestine. A healthy gut plays a crucial role in overall health, and one important aspect of gut health is gut permeability.
In this article, we will discuss the mechanism of gut permeability, nutrition to help it, factors that damage gut permeability, and diseases linked to it.
Mechanism of Gut Permeability
The intestinal lining is made up of a single layer of cells known as enterocytes. These cells are held together by tight junctions, which regulate the passage of nutrients, ions, and water from the intestine into the bloodstream. The gut has a selective barrier that allows the absorption of nutrients while preventing the entry of harmful substances, such as toxins and bacteria. However, certain factors can damage the tight junctions, leading to increased permeability and allowing unwanted substances to pass through the gut wall and into the bloodstream. When this happens it is term a “leaky gut”.
Nutrition to Help Gut Permeability
Several nutrients have been found to help support gut permeability, including:
Probiotics: Live bacteria that promote a healthy balance of gut bacteria and improve the integrity of the gut lining. A study conducted by Cao et al. found that a probiotic mixture improved gut permeability in people with inflammatory bowel disease (IBD).
Prebiotics: Non-digestible fiber that promotes the growth of beneficial gut bacteria. A study by Lopetuso et al. found that prebiotic supplementation improved gut permeability in people with IBD.
Glutamine: An amino acid that supports the growth and repair of intestinal cells. A study conducted by Wu et al. found that glutamine supplementation improved gut permeability in people with IBD.
Zinc: Zinc is used by the body to help the “tight junctions” in-between each cell of the gut wall.
You might be able to see that helping the gut heal is a lot about giving the body the nutrients that it can then use to heal itself.
There is a well known approach to healing the gut called the 4R program which I will go in to in another newsletter. It can be an approach Christian Bates would use in an Avatar Biotfeedback scan to help heal a gut issue.
Factors That Damage Gut Permeability
Several factors can damage gut permeability, including:
Poor diet: A diet high in processed foods, sugar, and unhealthy fats can damage the gut lining and lead to increased permeability.
Stress: Chronic stress can damage the gut lining and increase permeability.
During a biofeedback Avatar scan it can be determined which approach is best for YOU. For example it might be that you do need stress support first, rather than gut support. This is one of the best things that an Avatar scan provides, the order in which to start the healing process.
Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics, can damage the gut lining and increase permeability. A study by Bjarnason et al. found that NSAID use led to increased gut permeability in humans.
Diseases Linked to Gut Permeability
Several diseases have been linked to gut permeability, including:
Inflammatory bowel disease (IBD): A group of conditions characterised by chronic inflammation of the gut. Studies have shown that increased gut permeability is associated with the development and progression of IBD.
Celiac disease: An autoimmune disorder in which the ingestion of gluten leads to damage of the gut lining. Studies have shown that increased gut permeability is associated with the development of celiac disease.
Food allergy and intolerance: Studies have shown that increased intestinal permeability can lead to the passage of undigested food proteins and bacterial components into the bloodstream, which can trigger an immune response and lead to the development of food allergies and intolerances. Additionally, certain food components such as gluten and casein have been shown to also increase intestinal permeability .
Anxiety and depression: Studies have found that increased gut permeability can lead to the translocation of bacterial components into the bloodstream, triggering an inflammatory response that may contribute to the development of mood disorders. In one study, individuals with irritable bowel syndrome (IBS) were found to have increased gut permeability and higher levels of anxiety and depression compared to healthy controls.
In conclusion, gut permeability plays a crucial role in overall health, and certain nutrients can help support it.
For these reasons it is why the Hippocrates quote “All diseases begin in the gut” is such an incredible observation and remains such an important approach to health re-creation now.
The references for this Blog are at the bottom of the page.
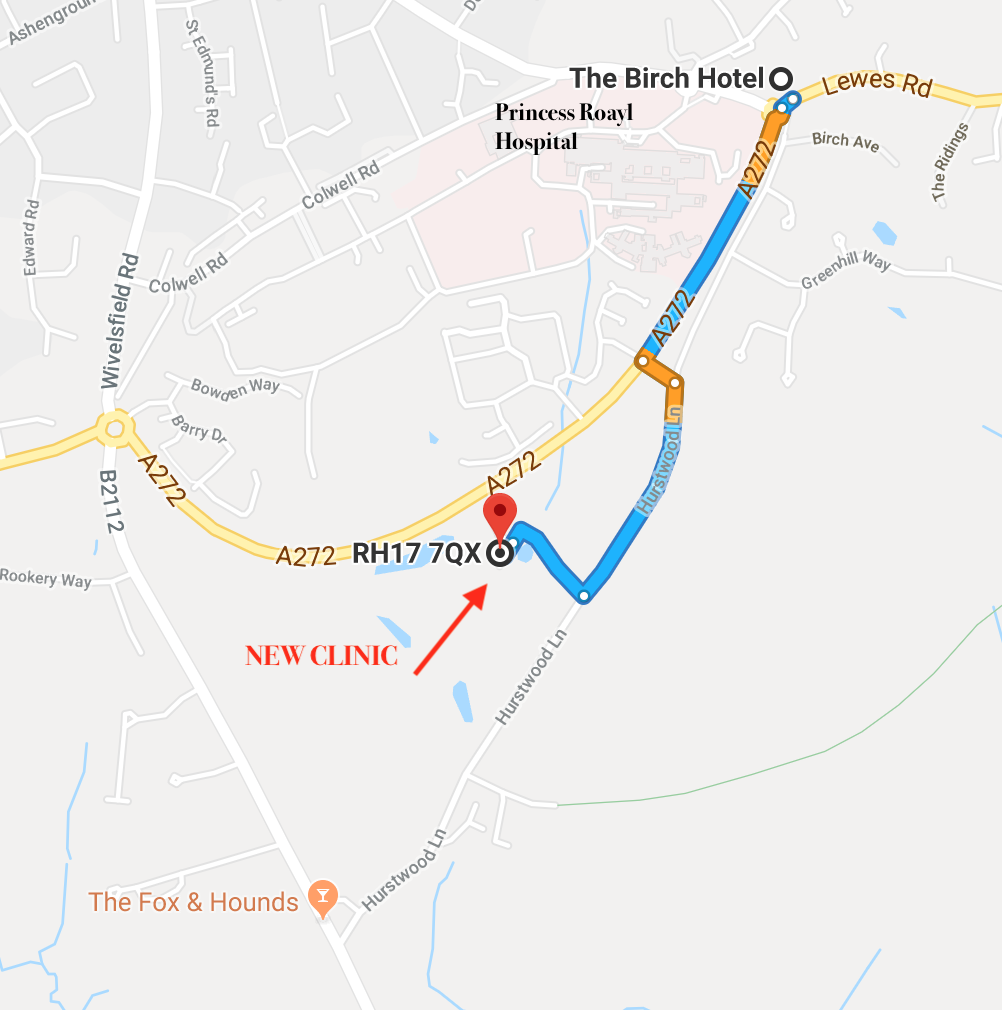
If you would like help using this type of approach to your health then have a look at this months special offer on an Avatar Biofeedback scan with Christian Bates which is below this articles. You will find a link to learn more about the Avatar scan and also the online purchase link for the special offer.
https://www.theperrymount.com/shop/#!/Avatar-BioFeedback-Scan-OFFER/p/591614241/category=156987147
References for this blog
Cao, Y., Shen, J., Ran, Z. H., & Guo, Z. (2014). Use of probiotics in the treatment of severe acute pancreatitis: a systematic review and meta-analysis of randomized controlled trials. Critical care, 18(1), R57. https://doi.org/10.1186/cc13806
Lopetuso, L. R., Scaldaferri, F., Franceschi, F., Gasbarrini, A., & Probiotics, P. (2018). The therapeutic management of gut barrier leaking: The emerging role for mucosal healing agents. European journal of pharmacology, 826, 115-117. https://doi.org/10.1016/j.ejphar.2018.02.019
Wu, G., Wang, B., Wei, H., Huang, J., & Cai, Y. (2010). Effects of dietary arginine and glutamine on intestinal health and immunity. Frontiers in bioscience (Landmark edition), 15, 1430-1441. https://doi.org/10.2741/3713
Desai, M. S., Seekatz, A. M., Koropatkin, N. M., Kamada, N., Hickey, C. A., Wolter, M., ... & Martens, E. C. (2016). A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell, 167(5), 1339-1353. https://doi.org/10.1016/j.cell.2016.10.043
Konturek, P. C., Brzozowski, T., & Konturek, S. J. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. Journal of physiology and pharmacology: an official journal of the Polish Physiological Society, 62(6), 591-599. https://www.ncbi.nlm.nih.gov/pubmed/22314561
Bjarnason, I., Williams, P., So, A., Zanelli, G. D., & Levi, A. J. (1984). Intestinal permeability and inflammation in rheumatoid arthritis: effects of non-steroidal anti-inflammatory drugs. The Lancet, 323(8385), 1171-1174. https://doi.org/10.1016/s0140-6736(84)92544-4
Fasano, A. (2012). Intestinal permeability and its regulation by zonulin: diagnostic and therapeutic implications. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 10(10), 1096-1100. https://doi.org/10.1016/j.cgh.2012.08.012
Arrieta, M. C., Madsen, K., Doyle, J., & Meddings, J. (2009). Reducing small intestinal permeability attenuates colitis in the IL10 gene-deficient mouse. Gut, 58(1), 41-48. https://doi.org/10.1136/gut.2007.144642
Clemente, M. G., De Virgiliis, S., Kang, J. S., Macatagney, R., Musu, M. P., Di Pierro, M. R., ... & Tron
Food allergy, intolerance and anxiety
References:
Fasano, A. (2012). Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiological reviews, 91(1), 151-175. https://doi.org/10.1152/physrev.00003.2008
Hollon, J., Puppa, E. L., Greenwald, B., Goldberg, E., & Guerrerio, A. (2015). Increased intestinal permeability in patients with celiac disease: a review of the literature. Advances in pediatrics, 62(1), 53-66. https://doi.org/10.1016/j.yapd.2015.02.003
de Theije, C. G., Wu, J., da Silva, S. L., Kamphuis, P. J., Garssen, J., Korte, S. M., ... & Kraneveld, A. D. (2011). Pathways underlying the gut-to-brain connection in autism spectrum disorders as future targets for disease management. European journal of pharmacology, 668, S70-S80. https://doi.org/10.1016/j.ejphar.2011.07.013
Maes, M., Kubera, M., Leunis, J. C., & Berk, M. (2013). Increased IgA and IgM responses against gut commensals in chronic depression: further evidence for increased bacterial translocation or leaky gut. Journal of affective disorders, 151(2), 612-618. https://doi.org/10.1016/j.jad.2013.06.032
Elsenbruch, S., Lucas, A., Holtmann, G., Haag, S., Gerken, G., Riemenschneider, N., ... & Schedlowski, M. (2006). Public speaking stress-induced neuroendocrine responses and circulating immune cell redistribution in irritable bowel syndrome. American Journal of Gastroenterology, 101(10), 2300-2307. https://doi.org/10.1111/j.1572-0241.2006.00772.x