Chances are that many of you may not have heard of insulin resistance or metabolic syndrome; however, this cluster of conditions and symptoms has become synonymous in the medical literature with dramatically higher risks for diabetes and heart disease.
According to the NHS, 3.7 million people have been diagnosed with type 2, lifestyle orientated diabetes and a further 12.3 million now meet the criteria for metabolic syndrome, which includes obesity, blood sugar dysregulation, insulin resistance, high blood pressure, elevated triglyceride levels, low HDL (the good cholesterol) and abdominal adiposity as the primary determining factors.
The fact that development of these metabolic misfortunes generally occurs insidiously over time and in tandem with prolonged stressors, often means that warning signs may not be apparent until morphed into full-blown disease.
Many people chalk weight gain in their 30’s and 40’s as a normal part of the aging process and to a certain degree this is true. There is an issue though with the type of weight gain. Visceral (around functional tissue and organs) fat is highly inflammatory and is a predictor of cardiovascular health outcomes. Too much visceral fat (even in thin people) is a predictor of disease.
But what makes this syndrome trickier to monitor in its progress is the fact that it has multiple causes and isn’t just the high carb, sedentary lifestyle. You need to have certain genes (so check your family history or do a genetic test) along with the diet and exercise that would trigger the expression of those genes that predispose you to type 2 diabetes or cardiometabolic syndrome. Sleep, relationships and stress also contribute to the disease progression and should all be assessed and managed.
Stress induced cortisol de-sensitises tissues to the beneficial actions of many different hormones, including the sex hormones (estradiol, progesterone, testosterone), thyroid hormones, growth hormone, and insulin. Shutting down the muscle's response to insulin, which signals the uptake of glucose for energy, leads to unhealthy, elevated levels of blood glucose. When blood glucose levels increase and there is either not enough insulin being produced by the pancreas, or if the insulin is not working properly, also known as insulin resistance, then this can ultimately lead to metabolic syndrome, diabetes and/or heart disease.
Early detection of insulin resistance and metabolic syndrome is a key to preventing obesity-driven disease.
In the UK it is not considered relevant to test insulin through the NHS as it can’t be treated with a drug, just through lifestyle and isn’t a disease marker itself, it is a predictor of pre-diabetes. But do you really want to get sick before undertaking the changes you need to be healthy?
Up until now, medical providers have needed to order a variety of individual tests to help patients with a diagnosis of insulin resistance or metabolic syndrome. Now, however, there are a number of functional tests at our disposal for both early detection or monitoring.
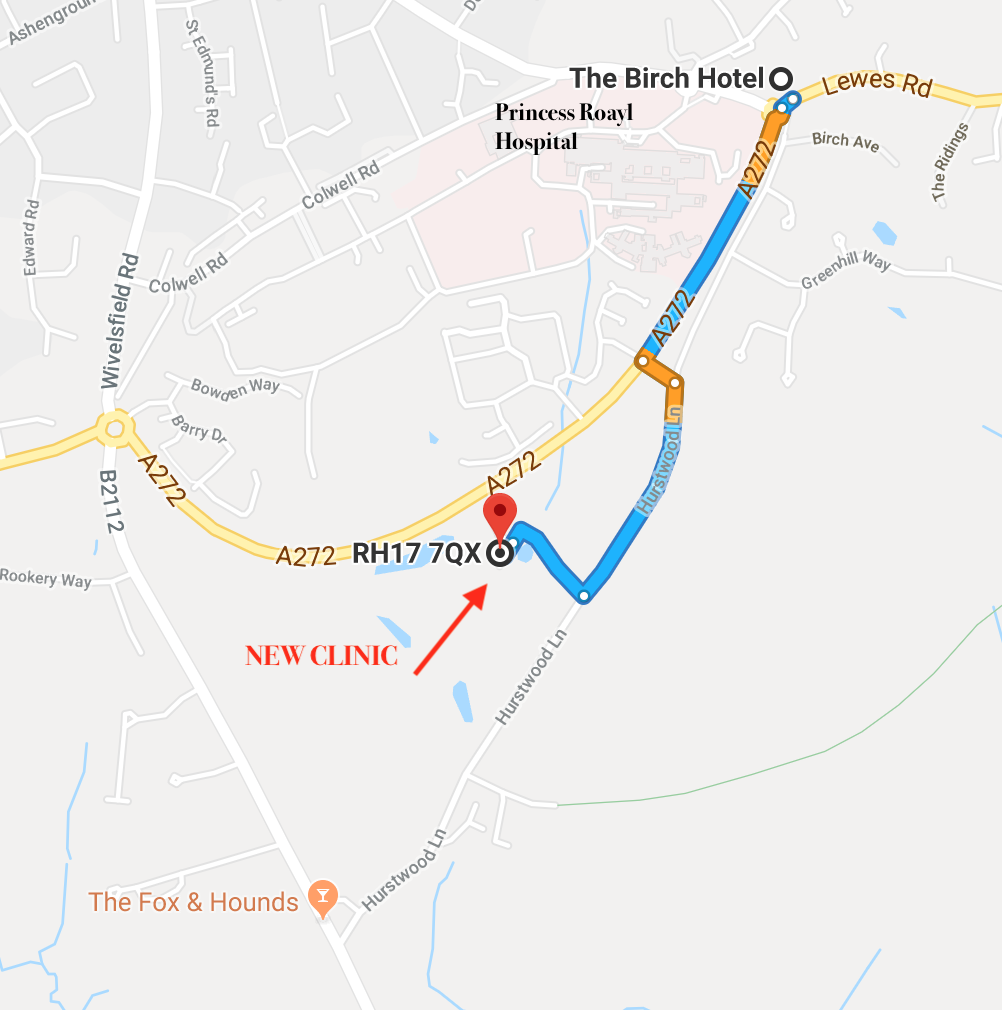
Early detection translates into disease prevention, yet it's estimated that only one in 10 people with pre-diabetes is aware. And just a quarter of those know that they can reduce their long-term health risks through early screening, lifestyle, and dietary improvements. Now is the time to take the opportunity to improve your health outcomes, call the Perrymount Clinic on 01444 410944 and screen yourself today!