When you think about health, you probably think about your heart, your muscles, or maybe your brain. But did you know there’s an invisible ecosystem inside you that has more impact on your health than nearly anything else?
It’s called the microbiome — and it’s absolutely essential for your digestion, immunity, metabolism, mood, and even longevity.
Today, let’s take a deep dive into what your microbiome really is, how it becomes imbalanced, and why science now links it to so many diseases.
What is the Microbiome?
Your microbiome is a community of trillions of microorganisms (bacteria, viruses, fungi, archaea, and protozoa) that live in and on your body.
The majority of them reside in your gut, particularly in the large intestine.
These microbes perform essential tasks for you, including:
- Breaking down food and producing short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate
- Producing vitamins such as B12, K2, biotin, and folate
- Training and regulating your immune system
- Maintaining the integrity of your gut lining (your barrier against toxins)
- Communicating with your brain via the vagus nerve and influencing neurotransmitters like serotonin
You can see the wide range of health benefits!
Which Bacteria Matter Most?
Researchers have identified some key groups of bacteria that dominate a healthy gut microbiome. These include:
Firmicutes — important butyrate producers that protect your gut lining
Bacteroidetes - help break down complex carbohydrates
Actinobacteria — essential in early life and immune development
Proteobacteria - (in small amounts) — some are normal, but overgrowth is linked to inflammation
A healthy gut is dominated by beneficial Firmicutes and Bacteroidetes with high diversity — meaning a large number of different species living together in balance.
What Does It Mean for the Microbiome to Be "Out of Balance"?
Scientifically, an imbalanced microbiome — called dysbiosis — is characterised by:
- Loss of diversity: Fewer types of bacteria present
- Overgrowth of harmful species: Such as Escherichia coli, Clostridium difficile, Klebsiella
- Depletion of beneficial bacteria.
- Inflammation and barrier dysfunction: Dysbiosis can damage the gut lining, leading to “leaky gut”
Think of a rainforest: A healthy microbiome is like a lush, diverse jungle. Dysbiosis is like a monoculture — dry, fragile, and vulnerable to disease.
Factors that drive dysbiosis include:
- Frequent antibiotic use
- Diets low in fiber but high in sugar and processed foods
- Chronic psychological stress
- Lack of exposure to nature and beneficial microbes
Diseases Linked to Dysbiosis
The research connecting microbiome imbalance to human disease is overwhelming. Dysbiosis has been associated with:
Digestive conditions: IBS, IBD, Crohn’s disease, ulcerative colitis
Metabolic disorders: Obesity, insulin resistance, type 2 diabetes
Mental health issues: Anxiety, depression, cognitive decline
Autoimmune diseases: Type 1 diabetes, rheumatoid arthritis, multiple sclerosis
Cardiovascular disease: Via production of inflammatory compounds like TMAO
Allergies and eczema: Especially in children exposed to antibiotics early in life
Neurodegenerative diseases: Alzheimer's and Parkinson’s disease
In short, the old quote “All diseases begin in the gut”, is continuously being scientifically proven years after it was observed.
The Good News: The Microbiome is Dynamic and Resilient
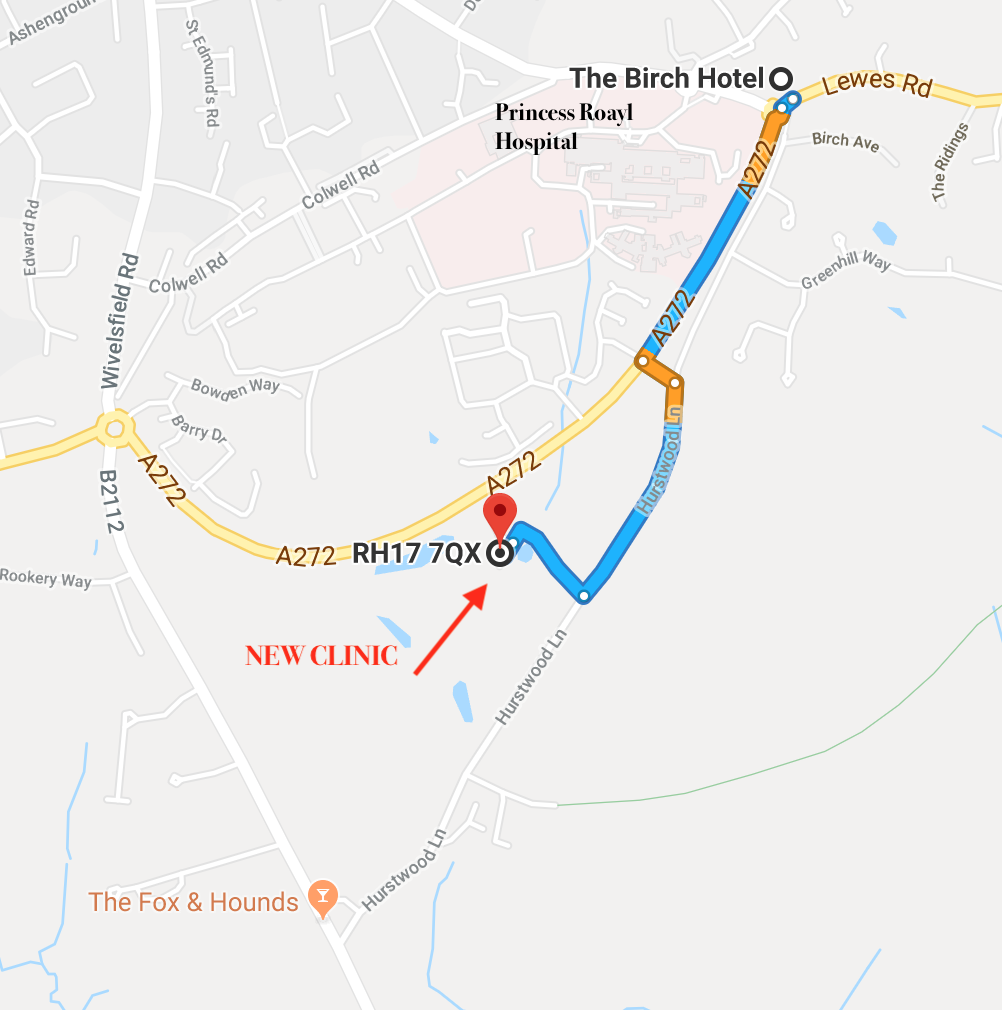
Even if your microbiome has been damaged by years of stress, poor diet, or medications, it can be improved to varying degrees using the 5R protocol which we focus on in our Bioresonance gut healing scan.
Learn more about our can here:
https://page.theperrymount.com/advancedhealthscan
More gut health newsletter are on the way! Stay tuned.
Prevention is better than cure.
The Perrymount Team.
References:
1. Koh A, et al. "From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites." *Cell*. 2016;165(6):1332-45.
2. Hill MJ. "Intestinal flora and endogenous vitamin synthesis." *European Journal of Cancer Prevention*. 1997;6(Suppl 1):S43-5.
3. Belkaid Y, Hand TW. "Role of the microbiota in immunity and inflammation." *Cell*. 2014;157(1):121-41.
4. Kelly CJ, et al. "Signals from the microbiota promote regulatory T-cell development." *Gastroenterology*. 2015;148(5):1001-11.
5. Cryan JF, et al. "The microbiota-gut-brain axis." *Physiological Reviews*. 2019;99(4):1877-2013.
6. Miquel S, et al. "*Faecalibacterium prausnitzii* and human intestinal health." *Current Opinion in Microbiology*. 2013;16(3):255-61.
7. Wexler HM. "*Bacteroides*: the good, the bad, and the nitty-gritty." *Clinical Microbiology Reviews*. 2007;20(4):593-621.
8. O'Callaghan A, van Sinderen D. "Bifidobacteria and their role as members of the human gut microbiota." *Frontiers in Microbiology*. 2016;7:925.
9. Shin NR, et al. "An increase in the *Proteobacteria* population in the gut microbiota of obese individuals." *Microbial Pathogenesis*. 2015;86:49-55.
10. Lozupone CA, et al. "Diversity, stability and resilience of the human gut microbiota." *Nature*. 2012;489(7415):220-30.
11. Buffie CG, et al. "Profound alterations of intestinal microbiota following a single dose of clindamycin results in sustained susceptibility to *Clostridium difficile*-induced colitis." *Infection and Immunity*. 2012;80(1):62-73.
12. Derrien M, et al. "*Akkermansia muciniphila* and its role in regulating host functions." *Microbial Pathogenesis*. 2017;106:171-81.
13. Camilleri M. "Leaky gut: mechanisms, measurement and clinical implications in humans." *Gut*. 2019;68(8):1516-26.
14. Manichanh C, et al. "The gut microbiota in IBD." *Nature Reviews Gastroenterology & Hepatology*. 2012;9(10):599-608.
15. Turnbaugh PJ, et al. "An obesity-associated gut microbiome with increased capacity for energy harvest." *Nature*. 2006;444(7122):1027-31.
16. Foster JA, Neufeld KA. "Gut–brain axis: how the microbiome influences anxiety and depression." *Trends in Neurosciences*. 2013;36(5):305-12.
17. Berer K, et al. "Gut microbiota from multiple sclerosis patients enables spontaneous autoimmune encephalomyelitis in mice." *PNAS*. 2017;114(40):10719-24.
18. Tang WHW, et al. "Gut microbiota in cardiovascular health and disease." *Circulation Research*. 2019;124(8):1183-96.
19. Arrieta MC, et al. "The intestinal microbiome in early life: health and disease." *Frontiers in Immunology*. 2014;5:427.
20. Sampson TR, et al. "Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease." *Cell*. 2016;167(6):1469-1480.e12.